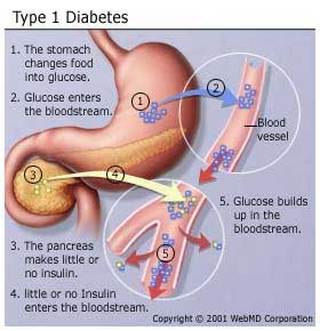
Diabetes mellitus type 1 (type 1 diabetes, T1DM, formerly insulin dependent or juvenile diabetes) is a form of diabetes mellitus that results from autoimmune destruction of insulin-producing beta cells of the pancreas. The subsequent lack of insulin leads to increased blood and urine glucose. The classical symptoms are polyuria (frequent urination), polydipsia (increased thirst), polyphagia (increased hunger), and weight loss.
Incidence varies from 8 to 17 per 100,000 in Northern Europe and the U.S. with a high of about 35 per 100,000 in Scandinavia to a low of 1 per 100,000 in Japan and China.
Eventually, type 1 diabetes is fatal unless treated with insulin. Injection is the most common method of administering insulin although other methods are insulin pumps and inhaled insulin. Other alternatives are Pancreatic transplants that have been used and also pancreatic islet cell transplantation. Transplantation is experimental yet growing.
Incidence varies from 8 to 17 per 100,000 in Northern Europe and the U.S. with a high of about 35 per 100,000 in Scandinavia to a low of 1 per 100,000 in Japan and China.
Eventually, type 1 diabetes is fatal unless treated with insulin. Injection is the most common method of administering insulin although other methods are insulin pumps and inhaled insulin. Other alternatives are Pancreatic transplants that have been used and also pancreatic islet cell transplantation. Transplantation is experimental yet growing.
Most people who develop type 1 are otherwise healthy. Although the cause of type 1 diabetes is still not fully understood, it is believed to be of immunological origin.
Type 1 can be distinguished from type 2 diabetes via a C-peptide assay, which measures endogenous insulin production.
Type 1 treatment must be continued indefinitely in all cases. Treatment should not significantly impair normal activities but can be done adequately if sufficient patient training, awareness, appropriate care, discipline in testing and dosing of insulin is taken. However, treatment remains quite burdensome for many people. Complications may be associated with both low blood sugar and high blood sugar, both largely due to the nonphysiological manner in which insulin is replaced. Low blood sugar may lead to seizures or episodes of unconsciousness, and requires emergency treatment. High blood sugar may lead to increased fatigue and can also result in long-term damage to organs.
Type 1 can be distinguished from type 2 diabetes via a C-peptide assay, which measures endogenous insulin production.
Type 1 treatment must be continued indefinitely in all cases. Treatment should not significantly impair normal activities but can be done adequately if sufficient patient training, awareness, appropriate care, discipline in testing and dosing of insulin is taken. However, treatment remains quite burdensome for many people. Complications may be associated with both low blood sugar and high blood sugar, both largely due to the nonphysiological manner in which insulin is replaced. Low blood sugar may lead to seizures or episodes of unconsciousness, and requires emergency treatment. High blood sugar may lead to increased fatigue and can also result in long-term damage to organs.
Signs and Symptoms

These symptoms may be the first signs of type 1 diabetes, or may occur when the blood sugar is high:
- Being very thirsty
- Feeling hungry
- Feeling tired or fatigued
- Having blurry eyesight
- Losing the feeling or feeling tingling in your feet
- Losing weight without trying
- Urinating more often
For other people, these warning symptoms may be the first signs of type 1 diabetes, or they may happen when the blood sugar is very high (see: diabetic ketoacidosis):
- Deep, rapid breathing
- Dry skin and mouth
- Flushed face
- Fruity breath odor
- Nausea or vomiting, inability to keep down fluids
- Stomach pain
- Headache
- Hunger
- Nervousness
- Rapid heartbeat (palpitations)
- Shaking
- Sweating
- Weakness
Exams and Test
Diabetes is diagnosed with the following blood tests:
- Fasting blood glucose level -- diabetes is diagnosed if it is higher than 126 mg/dL two times
- Random (nonfasting) blood glucose level -- you may have diabetes if it is higher than 200 mg/dL, and you have symptoms such as increased thirst, urination, and fatigue (this must be confirmed with a fasting test)
- Oral glucose tolerance test -- diabetes is diagnosed if the glucose level is higher than 200 mg/dL after 2 hours
- Hemoglobin A1c test
- Normal: Less than 5.7%
- Pre-diabetes: Between 5.7% and 6.4%
- Diabetes: 6.5% or higher
- When the blood sugar is higher than 240 mg/dL
- During an illness such as pneumonia, heart attack, or stroke
- When nausea or vomiting occur
- During pregnancy
- Check the skin and bones on your feet and legs.
- Check to see if your feet are getting numb.
- Have your blood pressure checked at least every year (blood pressure goal should be 130/80 mm/Hg or lower).
- Have your hemoglobin A1c test (HbA1c) done every 6 months if your diabetes is well controlled; otherwise, every 3 months.
- Have your cholesterol and triglyceride levels checked yearly (aim for LDL cholesterol levels below 70-100 mg/dL).
- Get yearly tests to make sure your kidneys are working well (microalbuminuria and serum creatinine).
- Visit your eye doctor at least once a year, or more often if you have signs of diabetic eye disease.
- See the dentist every 6 months for a thorough dental cleaning and exam. Make sure your dentist and hygienist know that you have diabetes.
Treatment
Because type 1 diabetes can start quickly and the symptoms can be severe, people who have just been diagnosed may need to stay in the hospital.
If you have just been diagnosed with type 1 diabetes, you should probably have a check-up each week until you have good control over your blood sugar. Your health care provider will review the results of your home blood sugar monitoring and urine testing. Your provider will also look at your diary of meals, snacks, and insulin injections.
As the disease gets more stable, you will have fewer follow-up visits. Visiting your health care provider is very important so you can monitor any long-term problems from diabetes.
You are the most important person in managing your diabetes. You should know the basic steps to diabetes management:
INSULIN
Insulin lowers blood sugar by allowing it to leave the bloodstream and enter cells. Everyone with type 1 diabetes must take insulin every day.
Insulin is usually injected under the skin. In some cases, a pump delivers the insulin all the time. Insulin does not come in pill form.
Insulin types differ in how fast they start to work and how long they last. The health care provider will choose the best type of insulin for you and will tell you at what time of day to use it. More than one type of insulin may be mixed together in an injection to get the best blood glucose control. You may need insulin shots from one to four times a day.
Your health care provider or diabetes nurse educator will teach you how to give insulin injections. At first, a child's injections may be given by a parent or other adult. By age 14, most children can give their own injections.
People with diabetes need to know how to adjust the amount of insulin they are taking:
DIET AND EXERCISE
People with type 1 diabetes should eat at about the same times each day and try to eat the same kinds of foods. This helps to prevent blood sugar from becoming too high or low. See also:
The American Diabetes Association and the American Dietetic Association have information for planning healthy, balanced meals. It can help to talk with a registered dietitian or nutrition counselor.
Regular exercise helps control the amount of sugar in the blood. It also helps burn extra calories and fat to reach a healthy weight.
Ask your health care provider before starting any exercise program. People with type 1 diabetes must take special steps before, during, and after intense physical activity or exercise. See also: Diabetes and exercise
MANAGING YOUR BLOOD SUGAR
Checking your blood sugar levels at home and writing down the results will tell you how well you are managing your diabetes. Talk to your doctor and diabetes educator about how often to check.
A device called a glucometer can read blood sugar levels. There are different types of devices. Usually, you prick your finger with a small needle called a lancet to get a tiny drop of blood. You place the blood on a test strip and put the strip into the device. You should have results in 30 - 45 seconds.
Keep a record of your blood sugar for yourself and your doctor or nurse. This will help if you have problems managing your diabetes. You and your doctor should set a target goal for your blood sugar levels at different times during the day. You should also plan what to do when your blood sugar is too low or high.
For more information, see: Managing your blood sugar
Low blood sugar is called hypoglycemia. Blood sugar levels below 70 mg/dL are too low and can harm you.
FOOT CARE
Diabetes damages the blood vessels and nerves. This can make you less able to feel pressure on the foot. You may not notice a foot injury until you get a severe infection.
Diabetes can also damage blood vessels. Small sores or breaks in the skin may become deeper skin sores (ulcers). The affected limb may need to be amputated if these skin ulcers do not heal or become larger or deeper.
To prevent problems with your feet:
PREVENTING COMPLICATIONS
Your doctor may prescribe medications or other treatments to reduce your chances of developing eye disease, kidney disease, and other conditions that are more common in people with diabetes.
Sources:
http://www.nlm.nih.gov/medlineplus/ency/article/000305.htm
http://en.wikipedia.org/wiki/Diabetes_mellitus_type_1
If you have just been diagnosed with type 1 diabetes, you should probably have a check-up each week until you have good control over your blood sugar. Your health care provider will review the results of your home blood sugar monitoring and urine testing. Your provider will also look at your diary of meals, snacks, and insulin injections.
As the disease gets more stable, you will have fewer follow-up visits. Visiting your health care provider is very important so you can monitor any long-term problems from diabetes.
You are the most important person in managing your diabetes. You should know the basic steps to diabetes management:
- How to recognize and treat low blood sugar (hypoglycemia)
- How to recognize and treat high blood sugar (hyperglycemia)
- Diabetes meal planning
- How to give insulin
- How to check blood glucose and urine ketones
- How to adjust insulin and food when you exercise
- How to handle sick days
- Where to buy diabetes supplies and how to store them
INSULIN
Insulin lowers blood sugar by allowing it to leave the bloodstream and enter cells. Everyone with type 1 diabetes must take insulin every day.
Insulin is usually injected under the skin. In some cases, a pump delivers the insulin all the time. Insulin does not come in pill form.
Insulin types differ in how fast they start to work and how long they last. The health care provider will choose the best type of insulin for you and will tell you at what time of day to use it. More than one type of insulin may be mixed together in an injection to get the best blood glucose control. You may need insulin shots from one to four times a day.
Your health care provider or diabetes nurse educator will teach you how to give insulin injections. At first, a child's injections may be given by a parent or other adult. By age 14, most children can give their own injections.
People with diabetes need to know how to adjust the amount of insulin they are taking:
- When they exercise
- When they are sick
- When they will be eating more or less food and calories
- When they are traveling
DIET AND EXERCISE
People with type 1 diabetes should eat at about the same times each day and try to eat the same kinds of foods. This helps to prevent blood sugar from becoming too high or low. See also:
The American Diabetes Association and the American Dietetic Association have information for planning healthy, balanced meals. It can help to talk with a registered dietitian or nutrition counselor.
Regular exercise helps control the amount of sugar in the blood. It also helps burn extra calories and fat to reach a healthy weight.
Ask your health care provider before starting any exercise program. People with type 1 diabetes must take special steps before, during, and after intense physical activity or exercise. See also: Diabetes and exercise
MANAGING YOUR BLOOD SUGAR
Checking your blood sugar levels at home and writing down the results will tell you how well you are managing your diabetes. Talk to your doctor and diabetes educator about how often to check.
A device called a glucometer can read blood sugar levels. There are different types of devices. Usually, you prick your finger with a small needle called a lancet to get a tiny drop of blood. You place the blood on a test strip and put the strip into the device. You should have results in 30 - 45 seconds.
Keep a record of your blood sugar for yourself and your doctor or nurse. This will help if you have problems managing your diabetes. You and your doctor should set a target goal for your blood sugar levels at different times during the day. You should also plan what to do when your blood sugar is too low or high.
For more information, see: Managing your blood sugar
Low blood sugar is called hypoglycemia. Blood sugar levels below 70 mg/dL are too low and can harm you.
FOOT CARE
Diabetes damages the blood vessels and nerves. This can make you less able to feel pressure on the foot. You may not notice a foot injury until you get a severe infection.
Diabetes can also damage blood vessels. Small sores or breaks in the skin may become deeper skin sores (ulcers). The affected limb may need to be amputated if these skin ulcers do not heal or become larger or deeper.
To prevent problems with your feet:
- Stop smoking if you smoke.
- Improve control of your blood sugar.
- Get a foot exam by your health care provider at least twice a year and learn whether you have nerve damage.
- Check and care for your feet EVERY DAY, especially if you already have known nerve or blood vessel damage or current foot problems.
- Make sure you are wearing the right kind of shoes.
PREVENTING COMPLICATIONS
Your doctor may prescribe medications or other treatments to reduce your chances of developing eye disease, kidney disease, and other conditions that are more common in people with diabetes.
Sources:
http://www.nlm.nih.gov/medlineplus/ency/article/000305.htm
http://en.wikipedia.org/wiki/Diabetes_mellitus_type_1


